Minimum DataBase
Case study: Glen
Courtesy of Yvonne McGrotty BVMS, CertSAM, DipECVIM-CA, MRCVS, Internal Medicine Consultant

Background information
Name: Glen
Age: 5 years
Breed: Shetland sheepdog
Gender: Male neutered
Main presenting reasons:
5-day history of anorexia, PUPD and lethargy
History:
Glen was presented with a 5-day history of anorexia and sporadic episodes of vomiting; vomitus contained bile. PUPD was also reported. Glen was fully vaccinated and had not travelled outside the UK.
Physical Examination:
On examination Glen was quiet and extremely weak. Mucous membranes were very pale, and he was tachycardic (HR= 160bpm) with a grade III/VI left sided basilar systolic murmur and narrow pulses. Halitosis was present. Peripheral lymph nodes were not enlarged, and abdominal palpation was unremarkable. He was normothermic. Systolic blood pressure was significantly increased (190mmHg).
Initial interpretation and diagnostic plan
Oxygen therapy was provided and wide bore intravenous access obtained. AFAST and TFAST scans were negative for free fluid.
Marked pallor was most likely to reflect anaemia and the priority was to confirm this and determine whether the anaemia was regenerative or non-regenerative. Regenerative anaemias are usually due to either haemorrhage or haemolysis while non-regenerative anaemias can be due to chronic renal disease or bone marrow disease. The priority in this case was to determine whether the anaemia was due to haemorrhage, haemolysis or other diseases.
PUPD can be associated with a wide variety of medical conditions- biochemical testing and urinalysis were likely to help narrow down the differential list.
Initial diagnostic tests included a minimum database (Haematology, Biochemistry, Electrolytes and Urinalysis).
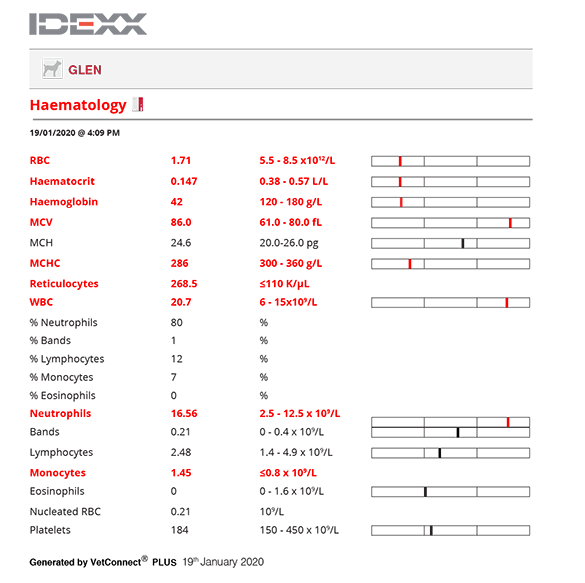
Haematology interpretation
A severe anaemia was confirmed (Ht= 14%) with an increase in reticulocytes consistent with regenerative response. Regeneration was confirmed on a blood film where there was strong evidence of polychromasia and anisocytosis. In addition, spherocytosis was present on the blood smear. An in-saline agglutination test was strongly positive which is pathognomonic for immune mediated haemolytic anaemia (IMHA).
Biochemistry interpretation
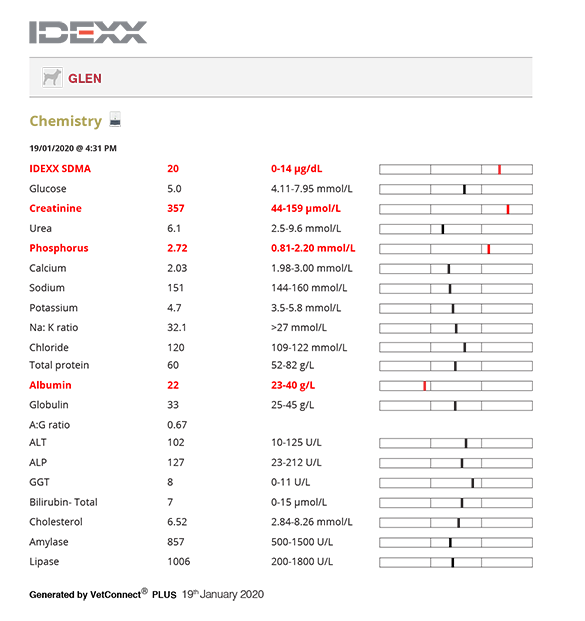
Azotaemia was present which along with increased SDMA and isosthenuric urine was consistent with kidney disease. Hyperphosphataemia here was secondary to decreased renal clearance. Hypoalbuminaemia was likely due to renal protein loss.
Electrolytes were unremarkable.
Urinalysis interpretation
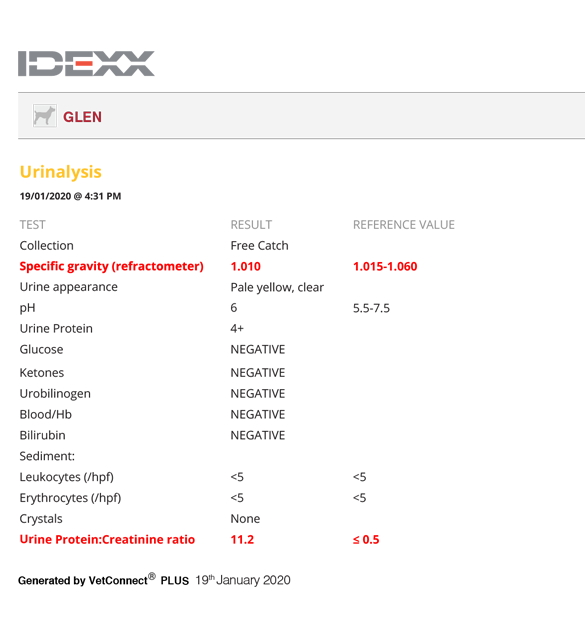
UPCR was markedly increased consistent with a severe protein losing nephropathy (PLN). Urine sediment was inactive and specific gravity was isosthenuric (1.010).
Further diagnostics
Blood typing confirmed that Glen was DEA 1.1 negative. Testing for infectious disease (Ehrlichia, Babesia and Leishmania) was considered but given the lack of travel history and lack of other suggestive signs, was considered unnecessary at this stage. A basal cortisol assay excluded hypoadrenocorticism.
Urine culture performed on a cystocentesis sample was negative. Renal ultrasound was unremarkable. Renal biopsies would have been necessary to confirm the underlying renal pathology, but Glen was certainly not a good candidate for anaesthesia and the therapeutic regime for this dog was unlikely to have been significantly altered by the results of renal biopsies.
Diagnostic tests
Haematology
Chemistry
Urinalysis
Diagnosis
Immune mediated haemolytic anaemia with IRIS stage ¾ chronic kidney disease, protein losing nephropathy and hypertension.
Outcome
Glen was transfused with DEA 1.1 negative packed red blood cells and immunosuppressive therapy initiated (prednisolone 1mg/kg PO q12h). As both agglutination and proteinuria were present, Glen had a high risk of thromboembolic disease so the antithrombotic agent clopidogrel (2mg/kg PO q24h) was also administered. An ACEi was initiated once the patient was more stable (starting dose benazepril 0.25mg/kg PO q24h), to reduce the level of renal proteinuria and the dose was titrated to effect. A renal prescription diet was offered, and a phosphate binder was added to the therapeutic regime a few weeks later when the renal diet alone failed to reduce the serum phosphate levels significantly. Hypertension was controlled with calcium channel blockers (amlodipine 0.05mg/kg PO q12h), which were titrated to effect.
Anaemia resolved with immunosuppressive therapy and prednisolone treatment was gradually tapered and withdrawn. UPCR improved with ACEi but did not return to reference range. Glen survived for a further year with excellent quality of life before succumbing to the effects of his renal disease.
In this case, the results of the Minimum Database led to a rapid diagnosis in a complicated case. This in turn resulted in prompt therapeutic intervention and a good outcome for Glen.