Minimum DataBase
Case study: Jasper
Courtesy of Robert White Adams MRCVS of Companion Care, Weston Super Mare

Background information
Name: Jasper
Age: 10 years
Breed: Collie
Gender: Male neutered
History and presenting reason
10yo MN Collie who presented with a 3-day history of pyrexia, lethargy and inappetence. He had not responded to NSAIDs and amoxicillin given at another practice the previous afternoon.
By the time he was seen at our practice he had not drunk for over 24 hours. His history yielded nothing further of note. Physical exam was a little limited due to poor patient cooperation, although pyrexia of 40.2°C was confirmed. All in all, not a lot to go on!
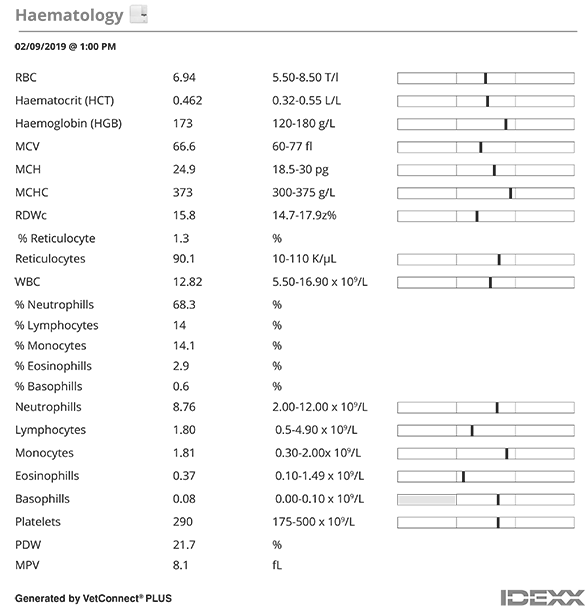
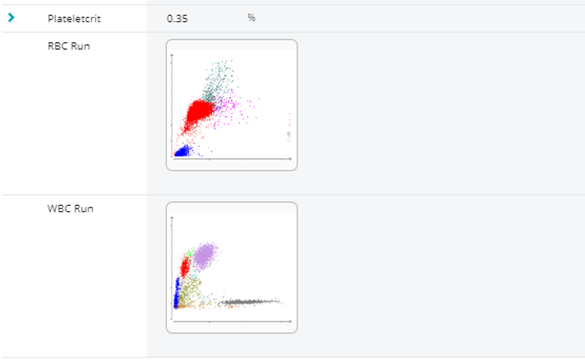
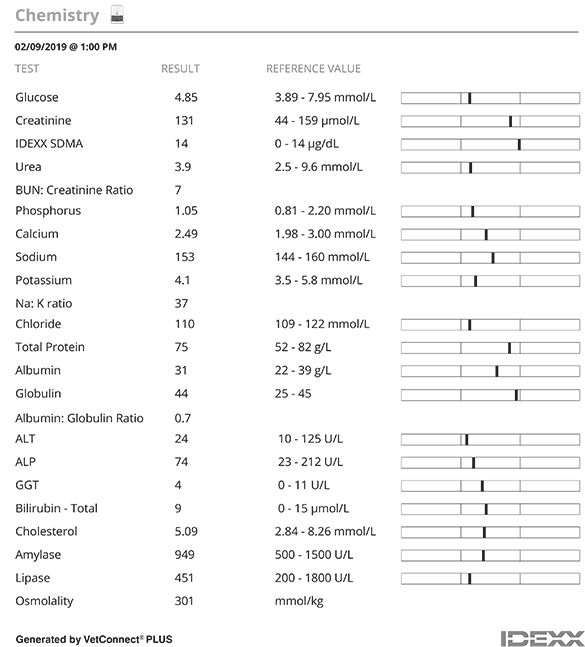
A Minimum DataBase consisting of haematology, Chem 17, SDMA and electrolytes and urinalysis) was performed. A dribble of urine showed a USG 1.045 and a standard biochemistry dipstick revealed no abnormalities.
Interpretation of results
Routine haematology (Lasercyte) was unremarkable, and a Chem17+Lytes, and SDMA (CatalystOne) profile was equally uninteresting.
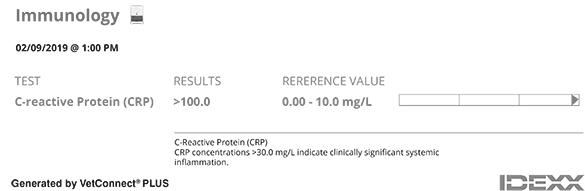
However, serum CRP was hugely elevated confirming that there was an inflammatory process going on.
We were concerned about dehydration setting in, but Jasper was too ‘unfriendly’ to tolerate IV fluid therapy without some degree of sedation. However, the decision was made to progress with sedation and carry out survey imaging whilst getting some fluids on board at the same time.
Radiographs were unhelpful and a survey abdominal ultrasound looked to be equally unrewarding until we got to the prostate (which I confess, since I was scanning a neutered dog, popped into my view a little by accident as I explored the caudal region of the bladder!) where a lovely cluster of small prostatic abscesses could be seen. Guided FNAs were taken from the prostate and a urinary catheter prostatic ‘wash’ sample was sent for both culture and cytology.
Jasper was given intravenous NSAIDs, enrofloxacin and paracetamol but as feared, after waking up, was intolerant (!) of hospitalization and fluid administration. Fortunately, he seemed bright enough to go home with oral versions of the same medications.
The following day, external laboratory reports for the FNAs confirmed abscessation; the cytology results showed no sign of malignancy on either sample. However, subsequent C&S results were non-diagnostic as nothing had grown on the bacterial culture samples. To confound matters, the advice I received was that prostatic infections, especially in neutered dogs, can be slow to improve, and often require long-sustained courses of antibiotics.
At re-examination a few days later, Jasper did appear brighter but was still anorexic. He had started to drink, and his temperature had gone down to 39.5°C. But here was the crux of the problem - was his mild improvement seen evidence that our treatment was working?... or was it just due to the palliative effects of NSAIDs and paracetamol? These questions were easily answered by repeat CRP testing. A second CRP test, 5 days after the first, showed serum levels of CRP had halved. Whilst the result was still outside the reference range there was a significant reduction which confirmed a positive response to therapy and treatment was therefore continued.
Over the next 3 weeks Jasper continued to improve slowly, but steadily. By day 10 his rectal temperature was normal, but whilst his CRP level was decreasing, it was still high. However, the ongoing trend of decreasing CRP results gave us confidence to persevere with treatment. It wasn’t until day 20 that Jasper’s owners reported he was back to normal, and a final CRP assay on day 22 was pleasingly normal too! Treatment was phased out over the following week, with no relapse of clinical signs noted. A final CRP sample taken two weeks later was still normal and it took us a while to find his now normal-appearing shriveled /neutered dog prostate on a repeat ultrasound scan.
CRP results contributed to the successful diagnosis, management and outcome of this case.
The initial elevated CRP result gave us the confidence to keep looking for an inflammatory cause of pyrexia, despite the absence of any other clinical, biochemical and haematological abnormalities. It was also invaluable for monitoring the response to treatment. The trend of decreasing CRP results meant we were able to differentiate a true reduction in pathology from just the effects of anti-inflammatory medication. It confirmed that we were doing the right thing by persisting with treatment.
Diagnostic tests